In many traditional trials, the primary endpoint is often selected based on understanding of what is known about how the intervention is thought to work. Sometimes that means that potentially important adverse effects are captured using secondary endpoints. That approach can work when you’re testing one drug, in one setting, at one point in time.... but it can also require application of judgement to determine the balance between beneficial and adverse effects of the intervention.
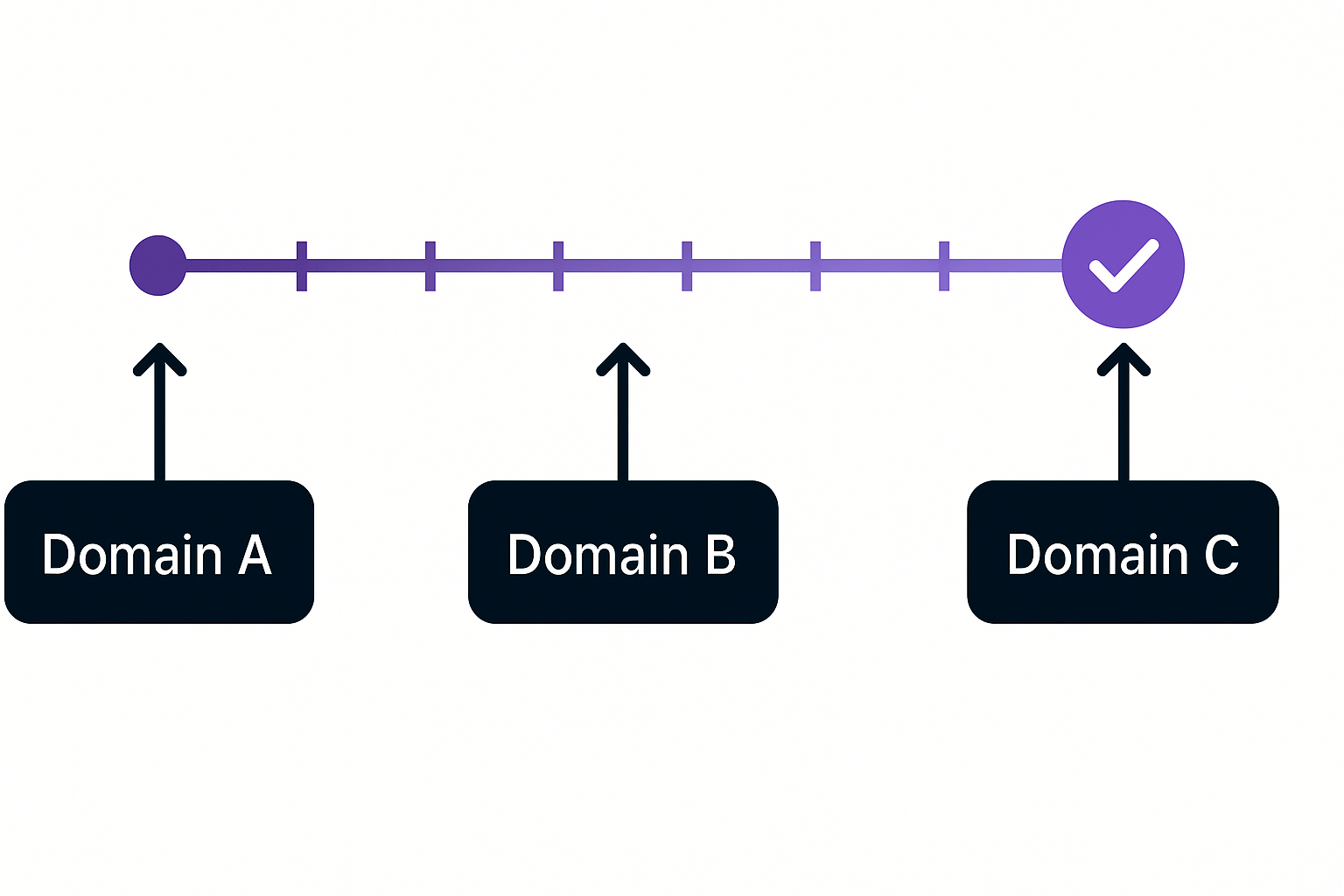
But what happens when the trial isn’t just one study – it’s one of many trials within a living platform, continuously expanding with new domains, treatments, and questions?
There are important operational reasons to have a single common endpoint in a platform. But, the act of having to choose a single common endpoint often leads to better thinking about what is really important for patients and clinicians, that will also be acceptable to regulators. In this situation the ideal endpoint is something universal that captures the aggregate effect of beneficial and harmful effects of an intervention that will be just as effective when applied across multiple different domains as the platform grows.
An ordinal scale comprising patient-centred components can provide that “common currency.” It doesn’t mean endpoints are changed on the fly, it means choosing one upfront that can carry the weight of evolution, expansion, and comparison.... and be something that is meaningful to patients with the disease.
The result? Evidence that is rigorous,credible, and comparable across interventions, conditions, and even patient groups, maximising the value of every patient who contributes to the trial.




.png)
.png)